Facts and Figures
- 1 in 10 women and those assigned female at birth in the UK of reproductive age live with endometriosis
- Endometriosis is the second most common gynaecological condition in the UK
- 10% of women and those assigned female at birth worldwide have endometriosis
Endometriosis is a long-term condition where tissue similar to the lining of the womb (uterus) starts to grow in other places, such as the ovaries and the fallopian tubes. The condition can cause pain that is sometimes debilitating (especially during menstrual periods). Fatigue, bowel, bladder and fertility problems may also occur. 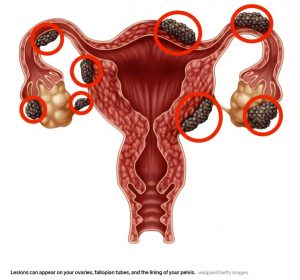
With endometriosis, the endometrial-like tissue acts the same way as the tissue in the womb; thickening, breaking down and bleeding with each menstrual cycle. Because this tissue has no way to exit, it becomes stuck. The hormonal changes of your menstrual cycle can cause the misplaced endometrial tissue to become irritated, inflamed and painful. The tissue will continue to grow, thicken and breakdown. Over time, the tissue that has broken down becomes trapped in your pelvis resulting in scarring, adhesions where tissue binds your pelvic organs together, extreme pain during periods and fertility problems.
The disease can affect women of any age, with 1 in 10 women of reproductive age suffering with this condition. Luckily, there are treatments to help manage the condition.
Symptoms of Endometriosis
The symptoms linked to endometriosis vary from case to case. Some women are badly affected, whereas others may not experience any noticeable symptoms. The most common symptom is pelvic pain, often associated with menstrual periods. You may also experience the following symptoms:
- Pain in your lower tummy or back, typically worse during your period
- Extreme period pain that prevents you from carrying out your daily activities
- Pain during or after intercourse
- Nausea, constipation, diarrhoea
- Difficulty getting pregnant
- Heavy periods (excessive bleeding)
The severity of your pain does not determine the extent of the condition. You may have mild endometriosis and experience severe pain, or you could have advanced endometriosis and be suffering with little to no pain.
Endometriosis can be mistaken for other conditions that can cause pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts. It can also be confused with irritable bowel syndrome (IBS), a condition that causes abdominal cramps, diarrhoea and constipation. IBS can be experienced alongside endometriosis, which can complicate the diagnosis.
It is important to seek medical advice if you experience any symptoms listed above. If your symptoms change following a diagnosis it is important to discuss these with your doctor. It is easy to relate all problems to endometriosis, but it may not always be the cause.
Causes of Endometriosis
Although the exact cause of endometriosis is unknown, possible causes include:
Retrograde Menstruation
In retrograde menstruation (when you have a period), menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of leaving the body through the vagina. The endometrial cells then implant themselves on the pelvic walls and surfaces of pelvic organs where they grow and continue to thicken and bleed throughout each menstrual cycle. It has been suggested that the majority of women experience some form of retrograde menstruation, but their bodies are able to clear the cells.
Immune Dysfunction
In some cases, a problem with the immune system may mean the body is unable to recognise and destroy endometrial-like tissue that is growing on the outside of the uterus. Many women that have endometriosis appear to have reduced immunity to other conditions. It is unclear whether this contributes to endometriosis or whether this is a result of the condition.
Genetics
There have been studies that suggest some families may be more prone to endometriosis, but the causes of this are unclear. If a woman’s mother or sister has the condition, the likelihood of her also developing endometriosis is increased.
Metaplasia
Metaplasia is the progression where one type of cell changes into a different kind of cell. Metaplasia typically occurs due to inflammation and allows cells to change to fit their surrounding circumstances to better adapt to their environment. In the case of endometriosis, metaplasia would explain how the endometriosis cells appear suddenly in areas such as the lungs and skin. It would also explain the appearance of endometriosis cells in women with no womb or in men who have taken hormone treatments.
Diagnosis of Endometriosis
Being diagnosed with endometriosis can take a long process, with a recent study showing there is now an average of 7.5 years between women first seeing a doctor about their symptoms and receiving a firm diagnosis. The symptoms of endometriosis are extremely similar to other common conditions so it is crucial to share as much information as possible with your doctor to achieve an accurate diagnosis.
Your doctor will ask about your symptoms and any personal or family history of endometriosis. A general health assessment may also be suggested to determine if there are any other signs of a long-term disorder.
Your doctor may carry out one or more of the following tests:
Physical Examination
During a physical pelvic examination, your doctor will feel your abdomen for any abnormalities, cysts or scars behind the uterus. It is generally not possible to feel small areas of endometriosis unless they have caused a cyst to form.
Ultrasound Scan
An ultrasound scan uses high-frequency soundwaves to generate images of the inside of your body. Your doctor will use a tool called a transducer to create images, either via a transvaginal ultrasound (via the vagina) or an abdominal ultrasound. Both types of ultrasound produce images of your reproductive organs. They are not an effective tool to rule out the disease; however, they can help your doctor identify any cysts related to endometriosis.
Magnetic Resonance imaging (MRI) Scan
An MRI scan is an examination that uses a magnetic field and radio waves to produce detailed images of the organs and tissues. In some cases, an MRI helps with surgical planning, providing your doctor with detailed information about the location and size of endometrial implants.
Laparoscopy
The only definite way to diagnose endometriosis is by a laparoscopy. A laparoscopy is an operation in which a camera (a laparoscope) is inserted into the pelvis via a small incision near the navel. The doctor uses the camera to see the pelvic organs and provide further information about the location, extent and size of the endometrial implants. Your doctor may take a sample of tissue (biopsy) for further testing. Often, with surgical planning, your doctor can treat endometriosis during the laparoscopy so that you only need to undergo one surgery.
Treatment of Endometriosis
If you have been diagnosed with endometriosis, your doctor will discuss possible treatment options with you. Currently, there is no cure for endometriosis. The treatment options available aim to reduce the severity of symptoms and improve the quality of life for women living with the condition. The form of treatment you receive for your condition will be agreed between you and your doctor. They will consider many different factors when working out the best treatment method for you, such as your age, your symptoms and the severity of endometriosis you have.
There is no specific recommended treatment for endometriosis although doctors do recommend trying conservative treatments first, opting for surgery if initial treatment does not work.
Treatment options for women living with endometriosis include surgery, hormone treatment and pain relief. Everyone reacts differently to treatment and your doctor will help you find the one that works best for you.
Pain Medication
Your doctor may suggest you take an over-the-counter pain reliever, such as the nonsteroidal anti-inflammatory drugs (NSAIDs) or ibuprofen to help relieve painful cramps.
Hormone Therapy
Your doctor may recommend hormone therapy with pain relievers if you are not trying to get pregnant. In some cases, additional hormones are effective in reducing or eliminating the pain of endometriosis. The rise and fall of hormones throughout the menstrual cycle causes endometrial implants to thicken, break down and bleed. Hormone medication may slow endometrial tissue growth and stop new implants of endometrial tissue. Hormone therapy is not a permanent solution for endometriosis and you may experience symptoms after stopping treatment.
Hormonal Contraceptives
Birth control pills, patches and vaginal rings help regulate the hormones responsible for the build-up of endometrial tissue every month. Using hormonal contraceptives can help reduce or even eliminate pain in some cases.
Gonadotropin-Releasing Hormone (GnRH) Agonists and Antagonists
These drugs block the production of oestrogen that stimulate the ovaries. Oestrogen is the hormone that is primarily responsible for the development of female sexual characteristics. Blocking the production of oestrogen stops menstruation and generates an artificial menopause. Taking a low dose of oestrogen or progestin alongside GnRH agonists and antagonists can help decrease menopausal side effects such as vaginal dryness, hot flushes and bone loss. The ability to get pregnant as well as menstrual periods should return when you stop taking the medication.
Conservative Treatment
Conservative treatment is for women who want to get pregnant or experience severe pain and hormonal treatments are not working. The aim of conservative surgery is to remove or destroy endometrial growths without damaging the reproductive organs.
Surgery
Laparoscopy, a minimally invasive surgery is used to visualise and diagnose endometriosis; it can also be used to remove the endometrial tissue. Your doctor makes small incisions in the abdomen to surgically remove the growths or to burn or vaporise them. Even in severe cases of endometriosis, the majority of cases can be treated with laparoscopic surgery. Following surgery, your doctor may recommend taking hormone medication to help ease the pain.
Fertility Treatment
Endometriosis can lead to difficulty getting pregnant and in some cases, infertility. If you are having trouble getting pregnant, your doctor may recommend fertility treatment. Fertility treatment ranges from stimulating your ovaries to make more eggs to in vitro fertilisation (IVF). Which treatment is right for you depends on your personal circumstances.
Hysterectomy (Last Resort Surgery)
In rare cases, your doctor may suggest a total hysterectomy as a final option if your condition does not improve with other treatments. Surgery to remove the uterus and cervix (a total hysterectomy) and ovaries (Oophorectomy) results in menopause that leads to an absence of hormones produced by the ovaries, which can improve endometriosis pain. You will be unable to get pregnant following a hysterectomy and may experience side effects from early menopause such as heart or blood diseases, especially if you have the surgery below the age of 35. Get a second opinion before agreeing to undergo surgery if you are thinking of starting a family.
Living with Endometriosis
Dealing with the pain of endometriosis can be a challenge for many reasons. You may miss days from school or work, you may have to avoid social events, or give up hobbies. This can all take a physical and emotional toll on your overall health. There are ways to help manage your pain and stress levels with lifestyle changes.
Maintain a healthy, balanced diet
Studies have shown a connection between endometriosis and diets that are lacking in fruits and vegetables and high in red meat. You should also avoid alcohol as much as possible, limiting yourself to one drink a day.
Exercise
Women who exercise may produce less oestrogen and often have lighter periods, which can help improve their symptoms of endometriosis over time.
Manage your Stress
Finding ways to manage stress can help minimise your symptoms. Whether it is through meditation, yoga or by simply creating time for self-care.
Alternative Therapies
Although there is not enough research to support the use of alternative therapies for endometriosis, in some cases women find relief from their symptoms. Natural alternative techniques include acupuncture, herbal medicine and massage. Talk to your doctor prior to carrying out any alternative therapy, especially if you are considering over-the-counter supplements.
Home Remedies
Warm baths and heating pads can help ease pelvic muscles, reducing cramping and pain.
If you are living with endometriosis or its complications, joining a support group for women with endometriosis or fertility problems may be helpful. Sometimes it can help to simply talk to other women who can relate to you and your experiences.
Outlook
Endometriosis is a chronic condition with no cure and no fully understood cause.
Effective treatments are available to help manage pain and fertility issues, such as medication, hormone therapy, and surgery. The symptoms of endometriosis generally improve after menopause.
Need Help?
Our Consultant Gynaecologists are highly experienced in diagnosing and treating women that are currently experiencing endometriosis, with our medical team and nursing staff offering support in a sensitive and caring manner at all times.
To make an appointment to see a Consultant Gynaecologist consultant, please contact the reservations team on 01233 364 036 or email ashford.info@onehealthcare.co.uk
One Ashford Hospital is located in Kent and is ideal for private, insured and NHS patients located in Ashford, Dover, Canterbury, Folkestone, Maidstone and all nearby areas.
Why Choose One Ashford Hospital
• Access to leading Consultants within 48 hours*
• Competitive fixed-price packages
• Modern purpose-built hospital
• Fast access to diagnostics including MRI, X-Ray and Ultrasound
• Private, spacious, ensuite rooms
• Specialist Physiotherapy and nursing teams
• Little waiting time for surgery
• Calm, dignified experience
*Dependent on Consultant availability
**Terms and conditions apply








 One Ashford
One Ashford One Hatfield
One Hatfield