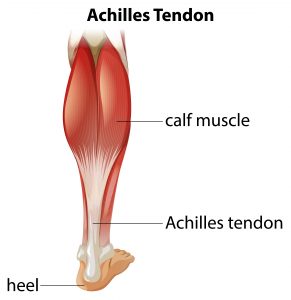
Achilles Tendinopathy is a painful condition affecting the Achilles tendon, the biggest and strongest tendon in the human body. It is a band of connective tissue that attaches the calf muscles to the heel bone, allowing you to lift your heel when you start to walk. It also helps you to walk, run or stand on tiptoe.
Causes of Achilles Tendinopathy
The primary cause of Achilles tendinopathy is overuse of the tendon. This occurs when the tendon is put under continuous stress, eventually developing small tears, resulting in degeneration. Without treatment, the tendon will become weaker as the tears are unable to heal on their own.
Athletes are prone to developing Achilles tendinopathy, in particular runners or those who participate in jumping activities, such as basketball and tennis.
Individuals who are overweight or obese are at a heightened risk of developing Achilles tendinopathy due to excess weight placed on many parts of the body, including the Achilles tendon.
As you become older, the Achilles tendon can become less flexible and is unable to cope with the strain.
Mr Bal Dhinsa, Consultant Orthopaedic Foot & Ankle Surgeon discusses Achilles Tendinopathy
You may also be at increased risk of developing the condition if you:
- Wear ill-fitting shoes, particularly ones that push on the back of the heel
- Have a high arched or low arched foot which can put stress on the tendon
- Have a family history of the condition
- Have previously injured the tendon or surrounding muscles
- Have a long-term health condition such as diabetes, arthritis or high blood pressure
- Have high cholesterol levels
- Are taking antibiotics belonging to the Quinolone group
Symptoms of Achilles Tendinopathy
Typical symptoms include:
- Pain in the back of the heel
- Swelling, tenderness and warmth around the tendon
- Difficulty walking
- A grating sensation
- A lump on the tendon
Pain can be intermittent, often feeling worse in the morning when you haven’t moved around for a while. It can also feel worse after certain activities and exercise.
Diagnosis
If you are experiencing any of the above symptoms, then book an appointment to see your GP or Physiotherapist who will be able to determine whether or not you have Achilles tendinopathy. They will begin by taking a full medical history and discussing your symptoms in order to rule out other related causes or conditions. It is important to provide as much information as you can, along with details of your exercise habits, regular activities and type of footwear you use.
Following this, they will perform a physical examination by examining your leg, ankle and heel. They may ask you to perform a series of movements or exercises to see how well you can move your leg. This can include squeezing your calf muscle to check the movement of your foot.
If your GP or Physiotherapist cannot diagnose Achilles tendinopathy from your symptoms alone, they may recommend an X-ray, Ultrasound or MRI scan to see if there are any tears. If tests show that you have torn your tendon, or your symptoms have lasted for more than 6 weeks, you will likely be referred to a specialist Orthopaedic Foot and Ankle Surgeon for the recommended treatment.
Treatment
Treatment options for Achilles tendinopathy range from conservative (non-surgical) methods to surgical procedures. If you believe you have injured your tendon, it is important to seek immediate medical advice as leaving it untreated can result in long-term damage.
Treatment will depend on the severity of your symptoms. The aim is to reduce strain on the tendon, preventing further injury and to allow it to repair. Non-surgical methods include:
- Applying ice-packs for 20 minutes an hour while the injury is still painful
- Over the counter painkillers such as paracetamol, ibuprofen or aspirin
- The use of orthotics (shoe inserts) to relieve pressure from the tendon, allowing it to heal.
Recovery can be slow and will depend on the severity of the injury and how well you follow the treatment advice given to you. If you are still experiencing pain after 6 weeks, your GP or physiotherapist may recommend any of the following if they feel they are suitable for you:
- Dry needling (this involves putting a thin needle into the tendon to trigger the healing process and strengthen the tendon)
- Extracorporeal shockwave therapy
- Platelet-rich plasma (PRP) injections. These use the individual’s own blood to help heal the tendon faster
- Low-level laser therapy
Steroid injections are not routinely recommended for the treatment of Achilles tendinopathy as there is inconsistent evidence on their effectiveness. The tendon can also rupture when the steroid is injected into it.
Surgical treatment may be recommended when all conservative options have failed, or your symptoms are too severe for them to have any positive effect. If your GP has suggested surgery, you will be referred to a specialist Foot and Ankle surgeon who will examine the condition of your tendon and discuss the surgical method to treat it. This may involve removing the damaged areas of the tendon and repairing the remains of it. This may involve using tissue from another one of your tendons, or from higher up the Achilles tendon.
Post-operative rehabilitation includes physiotherapy to stretch and strengthen the tendon. In most cases, people can resume their normal activities approximately 8-10 weeks following surgery, with a return to sporting activities around 3 – 6 months.
Prevention
There are a number of things you can do to help prevent Achilles tendinopathy. These include:
- Avoiding dramatic increases in sports training
- Incorporating stretching into your warm-up and cool-down routines
- Maintaining an adequate level of fitness for your sport
- Limit repetitive motions that overuse the tendon
- Wearing well-fitted supportive shoes, along with an orthotic if recommended
- Maintaining a healthy normal weight to reduce strain on the tendon
- Ensuring any underlying health problems are treated correctly
Need Help?
If you are experiencing pain in your foot or ankle and you think it could be Achilles tendinopathy, you can be seen by a Consultant Orthopaedic Foot and Ankle Surgeon at One Ashford Hospital, usually within 48 hours. One Ashford Hospital is well placed to see patients with knee injuries from Ashford, Maidstone, Canterbury, Folkestone, Dover and all surrounding villages. To book an appointment, call the hospital direct on 01233 364 022 or email here


 One Ashford
One Ashford One Hatfield
One Hatfield