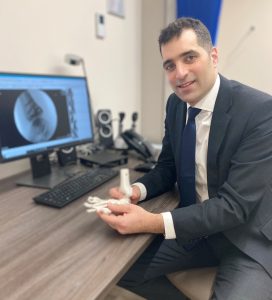
Heel pain is an extremely common condition, affecting one in eight people. Symptoms can range from mild to having a significant impact on daily life. Many conditions can contribute to heel pain, but the two most common causes are plantar fasciitis and Achilles tendonitis. We asked Mr Simon Mordecai, Consultant Orthopaedic Foot and Ankle Surgeon at One Hatfield Hospital to tell us more.
What is plantar fasciitis?
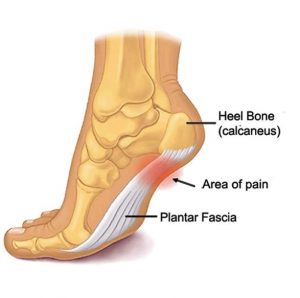
The plantar fascia is a thick band-like structure that runs from your heel bone to the base of your toes. It maintains your normal foot arch and absorbs load during activity. When this structure becomes inflamed, it causes pain at the bottom of your heel. This is known as plantar fasciitis.
What is Achilles tendonitis?
This is caused when your Achilles tendon, which connects your calf muscle to your heel, becomes inflamed causing pain at the back of the heel.
Who is likely to get heel pain?
Anyone can get heel pain, although commonly it tends to affect 40 to 60-year-olds and the younger athletic population. It can be as a result of wear and tear with gradual deterioration or, for younger athletes, because of repetitive overuse injuries. In both circumstances, tight calf muscles are an important factor and can cause excessive pressure on the Achilles tendon and plantar fascia.
What symptoms can I expect?
The pain is felt at the back or bottom of the heel. It is typically worse during the first steps in the morning or when getting up after sitting down for a long period of time. The pain then gradually subsides, as walking helps to stretch the Achilles and plantar fascia, but then returns after prolonged activity. There is often swelling around the heel.
How is it diagnosed?
This involves taking a thorough history and a full examination to determine the exact location and type of pain. You will likely require an ultrasound scan to assess the severity and sometimes an MRI scan, particularly for chronic cases.
How is it treated?
Heel pain can be a stubborn condition to treat and requires a combination of approaches. As a first-line treatment, I always advise calf stretching exercises supervised by a physiotherapist, in combination with heel cushions and arch supports. Any aggravating activities should be avoided until the pain subsides.
If this fails, then other treatments I offer are:
Extracorporeal shockwave therapy: Low energy sound waves cause a mechanical stimulus to the injured area, inducing microdamage and, in turn, stimulating a healing response. The treatment takes five minutes and requires three sessions, one to two weeks apart. You might experience mild discomfort during the treatment and often, symptoms are made a little worse before they get better.
Injection therapy: Steroid injections may be used to reduce pain and swelling around your heel depending on your condition. Alternatively, I might recommend a PRP (platelet-rich-plasma) injection. This involves taking a sample of your own blood, spinning it in a centrifuge machine to separate out the platelets and other healing factors, and then injecting it around the areas of pain. A course of three injections are usually required.
Surgical release: Often, ongoing heel pain is a result of tight calf muscles which fail to improve with conservative measures. In this instance, I would recommend a surgical release. This involves a minimal incision at the back of your knee to release the calf muscle. It is performed as a day case procedure and recovery is usually within two weeks.
How can I find out more?
Mr Mordecai specialises in all foot and ankle conditions including arthritis, sports injuries, bunions, heel pain, lesser toe problems, Morton’s neuroma, ingrown toenails and trauma. Mr Mordecai has regular clinics at One Hatfield Hospital.
Call 01707 443 333 to book a consultation with Mr Mordecai at One Hatfield Hospital.



 One Ashford
One Ashford One Hatfield
One Hatfield