Mr Bal Dhinsa, Consultant Orthopaedic surgeon at One Ashford Hospital discusses plantar fasciitis and management and treatment for the condition.
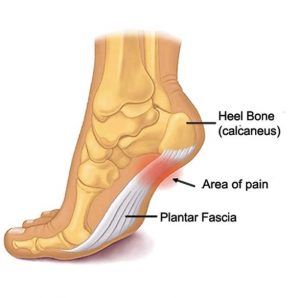
Plantar fasciitis is a common cause of heel pain. It is inflammation of the sheet of tissue (plantar fascia), that forms the arch of the foot, going from the heel to the toes. It results from overuse or being overstretched, causing inflammation and micro-tears. It can occur after a recent change in footwear or activities.
What are the typical symptoms?
Pain is typically described as a stabbing pain under the foot and heel. Patients often complain of pain when starting to weight-bear, it can then ease off with more weight-bearing (as it stretches) but returns with prolonged weightbearing (overuse).
How is Plantar Fasciitis managed?
Non-operative management
In my experience, most plantar fasciitis will settle with a combination of initial measures including analgesics, non-steroidal anti-inflammatory medication and stretching exercises. The stretching exercises may be plantar fascia specific stretching exercises alone, or in combination with calf stretching. The key to success is compliance with the stretching regime.
Night splints may also be utilised to keep the fascia stretched – this prevents the plantar fascia from returning to its normal resting position at night which becomes painful when stretched in the morning. However, I find compliance with this poor as it is quite uncomfortable for the patient and therefore do not routinely utilise this.
If despite these measures, there has been little benefit, I do suggest extracorporeal shock wave therapy in combination with further stretching as evidence suggests combination treatment has better outcomes. Shockwave therapy transmits high frequency shockwave impulses to the area of inflammation. This helps break down the scarring that is often present with inflammation and allows the stretching exercises to be carried out effectively.
If symptoms remain or return, the next step is to consider needling of the fascia and injection with corticosteroid. I perform this procedure under sedation in an operating theatre as the needling can be quite painful. During this procedure I use a hypodermic needle to scratch the scarred plantar fascia off its insertion to help break it down to allow stretching. Corticosteroid is also administered after the needling to help reduce inflammation. The key to this is that the needling allows stretching; however, without regular stretching the problem will return.
Operative management
From my experience, I find operative intervention for plantar fasciitis provides a guided outcome and therefore I try more predictable non-operative measures routinely. If surgical intervention is required due to non-resolving symptoms, despite non-operative management, I will discuss the specific risks associated with the surgery.
If the plantar fascia pain is an isolated problem, the procedure involves an incision on the inner aspect of the back of the heel to release the plantar fascia and release a nerve that is often entrapped.
In the situation where there is tight calf musculature, surgery may be suggested to alleviate this if stretching has not worked, and this has a more predictable outcome associated with higher patient satisfaction.
Rehabilitation
You will find your foot in heavy bandaging and a walking boot will be applied before you go home. You will be provided with crutches for support, and you will be permitted to weight-bear in the boot. Elevation, as much as possible, is important in the first few weeks. This boot will be removed in 2 weeks’ time for a wound check and physiotherapy will be started.
Complications
As with any surgery there are potential risks. This will be discussed in more detail during the consultation, however common complications are stiffness, swelling, nerve injury, infection, failure for symptoms to settle and irritation from the wound.
Can the plantar spur be removed?
I am often asked to see patients to consider removal of their plantar spur. This is not something I routinely perform, as evidence suggests that whilst a spur is suggestive of plantar fasciitis it is not causative for the symptoms and removal does not resolve symptoms. In fact, many patients without plantar fasciitis also have spurs present on X-ray.
The role of Platelet-rich plasma (PRP) injections
This is something I also frequently get asked about. There is little evidence for their benefit at the moment. Whilst it cannot be discounted, there is very little evidence available at the moment to recommend its use.
If you are struggling with plantar fascia pain and would like to book an initial consultant with Mr Bal Dhinsa, you can contact the hospital on 01233 423 000, or email ashford.info@onehealthcare.co.uk.
Mr Bal Dhinsa
Baljinder (Bal) Dhinsa is a fellowship trained Consultant Orthopaedic Surgeon, specialising in the treatment of foot and ankle conditions. On completion of Higher surgical training on the Southeast Thames rotation he completed British Orthopaedic Foot and Ankle Surgery (BOFAS) approved fellowships at Guy’s and St Thomas’ hospital and Malawi.
For more information on Mr Bal Dhinsa, please click here
Why Choose One Ashford Hospital
• Access to leading Consultants within 48 hours*
• Competitive fixed-price packages
• Modern purpose-built hospital
• Fast access to diagnostics including MRI, X-Ray and Ultrasound
• Private, spacious, ensuite rooms
• Specialist Physiotherapy and nursing teams
• Little waiting time for surgery
• Calm, dignified experience
*Dependent on Consultant availability
**Terms and conditions apply

 One Ashford
One Ashford One Hatfield
One Hatfield