Mr Robert Hone, Consultant ENT Surgeon at One Ashford Hospital gives a comprehensive insight into the thyroid, its function and common thyroid disorders.
The thyroid gland is found in the neck below the voice box and is shaped like a butterfly with a left and right side wrapping around the windpipe. It controls the body’s metabolism. Thyroid enlargement can occur due to general swelling or secondary to nodules (lumps), cysts or cancer.
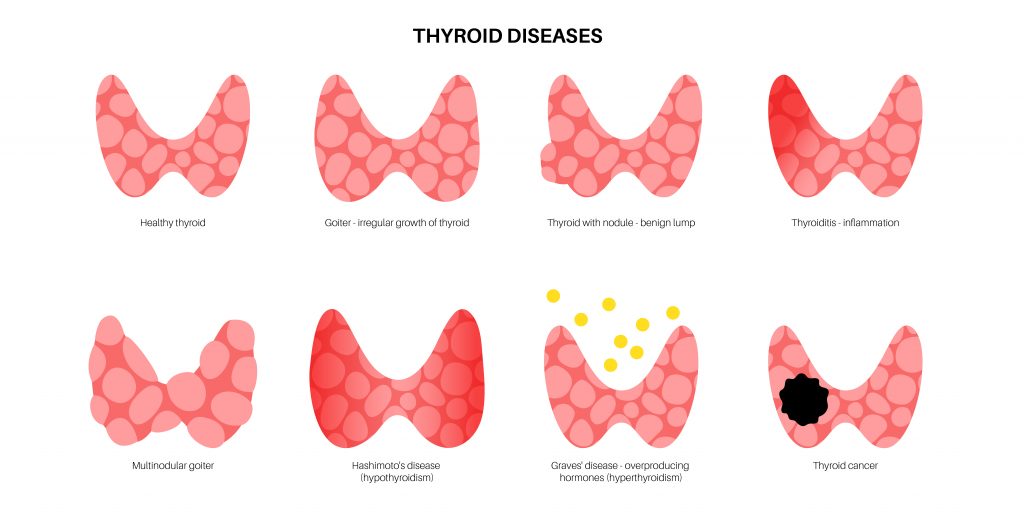
A thyroid goitre is the diffuse enlargement of the thyroid gland and can affect half or all of the thyroid gland. There are multiple causes for a diffuse goitre including hypothyroidism, hyperthyroidism, iodine deficiency, multiple nodules or cysts and autoimmune disorders. It can also occur during times of increased metabolism such as in puberty and pregnancy. A benign goitre does not necessarily require treatment unless you are suffering with compressive symptoms such as neck tightness, a feeling of pressure or choking when lying on your back; problems swallowing or very rarely breathing difficulties. If causing difficulty in breathing, the picture would be similar to asthma on spirometry (a test used to estimate the resistance of the lungs). Patients may also wish to have treatment for cosmetic reasons if they do not like the appearance of the swelling in the neck. Depending on the size and location of the goitre it can be treated conservatively; half of the thyroid removed (a hemithyroidectomy) or all the thyroid removed (a total thyroidectomy). Patients who have persistent symptoms of hyperthyroidism despite a course of medical treatment can be offered a total thyroidectomy to treat hyperthyroidism. Patients with hyperthyroidism should been seen and treated by Endocrinology before consideration of surgery.
Thyroid cancer is increasing in incidence and is the most common endocrine (a gland that produces hormones into the body) cancer. Thyroid cancer occurs in around 9 per 100,000 people and there are 5 subtypes. Thyroid cancer is usually present with a painless swelling in the anterior neck or due to a metastatic lymph node. It is rare for the cancer to present with pain, dysphonia or dysphagia. The prognosis for thyroid cancer is usually excellent with over 95% of people still alive 20 years following the diagnosis and treatment, although some types are more difficult to treat.
Any thyroid lump should undergo investigation. The basic investigations required include thyroid function tests and an ultrasound scan. Ultrasounds assess the appearance of the thyroid gland and if there are any nodules. According to the British Thyroid Association guidelines, the thyroid is graded on ultrasound in a U classification ranging from 1-5. The U classification is outlined below:
- U1 is benign and a normal thyroid gland.
- U2 is a benign thyroid nodule.
- U3 is indeterminate and if under 1 cm in size should have a repeat ultrasound in 6 months to assess for growth while those over 1 cm should have a fine needle aspiration cytology. U3 nodules over 1 cm should be referred on the 2-week wait rule while those under 1 cm could be managed with a repeat ultrasound or referred on the 2-week wait rule.
- U4 nodules are suspicious and should undergo FNA. U4 nodule should be investigated on the 2-week wait pathway and referred to the thyroid multidisciplinary team meeting.
- U5 is a cancerous nodule and should undergo FNA. These patients should be investigated on the 2-week wait pathway referred to the thyroid multidisciplinary team meeting referred to the thyroid multidisciplinary team meeting.
Fine needle aspiration cytology is where a needle is inserted into the thyroid nodule to collect some cells to sample the lump. It is done under ultrasound-guidance and is graded on the British thyroid Association guidelines as thy 1-5. The individual classifications are outlined below:
- Thy1 is non-diagnostic and therefore may need to be repeated.
- Thy2 is used for benign cytology.
- Thy3 is indeterminate and anything thy3 thyroid FNA should be discussed at the thyroid MDT with a referral on the 2-week wait pathway. Thy 3 a cytology can be sub-categorised into thy3a and thy3f which have a roughly 20% and 30% chance of malignancy respectively.
- Thy4 is suspicious for cancer.
- Thy5 is a confirmed malignancy.


 One Ashford
One Ashford One Hatfield
One Hatfield